In recent years, Artificial Intelligence (AI) has emersed itself into our lives through simple features such as autocomplete on our smartphones, pop-up advertisements based on our Google searches, and automatic light activation when we enter our homes. Likewise in a business context, AI plays a significant role in sectors such as the automobile, banking, insurance and life sciences, to name a few.
In machine learning, computers learn from datasets instead of being explicitly programmed with instructions. Deep learning is a type of machine learning that uses a layered artificial neuronal network and mimics the functioning of the human brain to generate automatic predictions from datasets.
Most of these involve in silico/computer-based validation, which takes data from retrospective studies and generates a hypothesis that can be tested prospectively and supported. Deep learning has reached new heights with the recent accomplishments in many areas of medicine, from diagnosing cancer to predicting suicide.
The healthcare sector is a challenging sector to be digitalised due to the mountain of information required to train the algorithm. Technological advances in this field have made great strides starting from video calls with doctors to computer algorithms for diagnosis.
The smartphone has become the hub of digitalisation in the new era of medicine even though there are a few challenges and limitations, AI has largely been positive.
This insight focuses on how AI can be used as well as challenges faced in the field of healthcare.
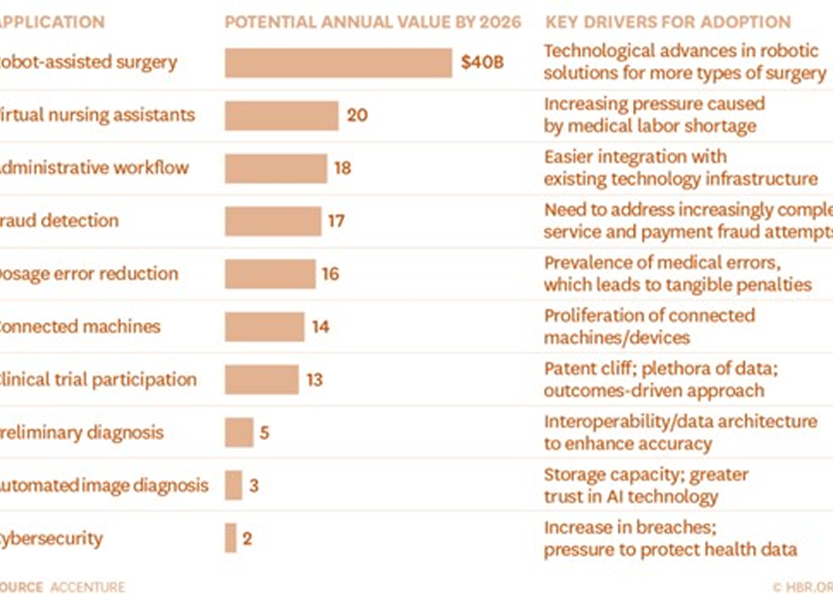
The chart below highlights the areas which can be targeted by AI and potential annual value that could be saved by 2026:
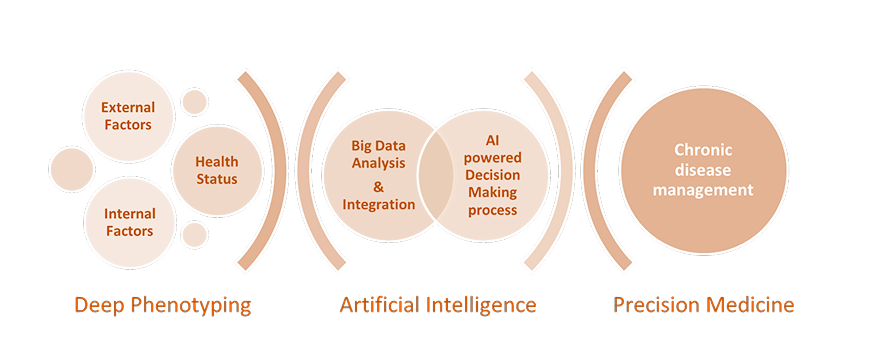
Precision medicine is focused on defining the molecular profile of an individual’s physiological status. Many internal and external factors can influence physiological changes and define the individual’s risk of a disease.
External factors such as diet, lifestyle, sleep, stress, socioeconomic status, geography, early life experiences and physical activity combined with internal factors relating to genetic background, gut microbiome, metabolism, inflammatory status are all critical factors in determining the individual’s health and disease risk profile.
Artificial Intelligence has been widely used to predict diseases when there’s a lack of obvious symptoms; chronic conditions like hypertension or diabetes might lead to conditions such as kidney disease. A study of 300,000 patients, demonstrated that AI accurately predicted these conditions.
AI Screening has had a marked impact on the diagnosis of Diabetic retinopathy, a leading cause of blindness, as wells as predicting if a person’s cells will become cancerous later on in their life. Interestingly, it is also now possible to scan the genes for any mutations and alter diet to alleviate the symptoms it causes.
To combat chronic conditions like diabetes, companies have developed algorithms that provide virtual coaching services to achieve optimal control and management as well as glucose sensors and smartphone apps for advanced diabetes management. For example, blood sugar levels can be monitored using smartphone AI recognition of food and meals, continuously monitoring glucose data and combining it with physical exercise data to provide coaching via texts.
Another example would be where a foot scanner takes images of the patient and, using machine learning, can detect diabetic foot ulcers. Algorithms can provide remote monitoring of an individual’s glucose measurements and guide his/her diet, exercise and dosage of medications.
Cardiovascular care is now possible at home for patients using remote monitoring with the help of companies like Tricog Health for cloud-based heart condition diagnosis. Recently, “wellness programs” have come to the limelight which target step-counting and blood pressure readings along with the results of lab tests to promote the importance of a healthy lifestyle.
Machine learning, a subtype of Artificial Intelligence has gained extraordinary momentum since the 1990s, especially in the space of genetic engineering.
There are two main applications of machine learning in Genetics:
1. Identification of harmful genes / mutated genes
Analysis of DNA is very complex (with more than 20,000 genes)and can become extremely tedious and time-consuming. Algorithms help to identify the mutated genes by comparing the person’s DNA with a normal one. Additionally, 3D imaging can be used to identify genetic mutations without the need to collect tissue samples through surgery.
2. Treatment of disease
A major argument in favour of gene editing is the ability to cut out disease-causing genes. Machine learning algorithms can help carry it out efficiently and precisely to assist DNA repair, thereby eliminating any potential for error. Similar to diagnosing disease using a genomic basis, AI can help identify which genes have been affected by harmful mutations and be targeted in gene therapy.
Although AI doesn’t replace the role played by scientists, it helps them visualise things and make it easier for them to sift through rich data sets easily (especially genomics).
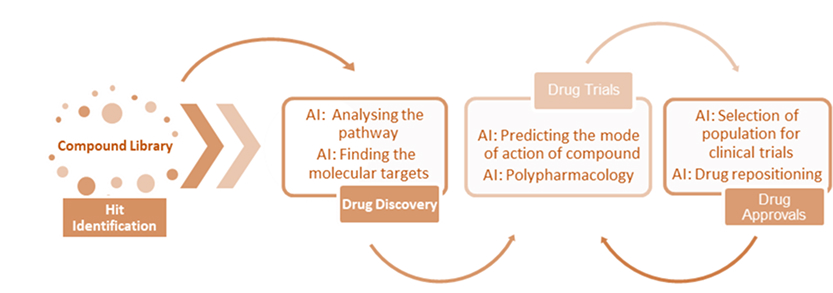
AI library screening and Automated AI molecule design result in faster development of more potent molecules and reduces the need for preclinical animal testing. In addition to identifying potential therapeutic molecules, it also eliminates those compounds which are already patented. Taking it to the next level is image processing through algorithms and automated microscopes to interrogate high-throughput drug testing of human cells to provide detailed information about the size and shape of cell and nuclei. The advantage of this automated drug discovery is the reduction in the number of compounds to be tested, as well as, predicting the right dose for experimental drugs. Drug discovery timelines can be reduced by around four years and efficiency improved by 60%.
Efforts of AI in Neuroscience are well underway to recapitulate the functioning of the human brain in computers. Even though there are many constraints for lab work to be automated, AI is being used to design the next set of experiments which can expedite the process efficiently.
Variability, ethical issues and cost play a significant role in clinical trials. In silico dataset is used to train the drug development algorithm by modelling biological systems during clinical trials and with hospital database. This approach has the potential to replace animals and humans and produce ‘virtual patients’. Some areas like paediatric and orphan disease trials can take advantage of in silico clinical trials.
Virtual care is gaining importance in the present age, as many patients are keen to remain in the comfort of their own homes without the risk of acquiring infections. Popularly known as ‘touchless warmth’, this concept of remote monitoring is replacing regular hospital rooms.
The hi-tech AI surveillance algorithm can warn and alert the clinician of the possibility of any conditions that could be developed despite the absence of any symptoms. Sensors and algorithms can detect/monitor the temperature, pulse, mood, activities and even the event of an elderly person falling over at home.
For these devices to be approved for home use by regulatory authorities, it needs to be proved that they are automatic, accurate, inexpensive and integrate well with remote monitoring facilities.
Healthcare in the form of a ‘Virtual Medical Assistant’ is gaining popularity owing to its ease of use. There are more than 250 million visually impaired people in the world and AI voice platforms give them unlimited help in their daily activities including promoting health or better management of a chronic condition.
Nowadays watchbands relay a person’s heart rate and physical activity to enable an electrocardiogram (ECG) to be used to look for any evidence of atrial fibrillation and alert the patient through messages.
Even though AI chatbots cannot provide the human touch and care, they can interact with aesthetically pleasing avatars – to empower not just physicians but also patients.
Having said this, Hiroshi Ishiguro has created bots with stunning human facsimile, including a remarkable similarity to human hands, which have built-in AI sensors to even detect a person’s mood and engage in at-a-stretch conversation for twenty minutes.
One of the major challenges that hospitals face is the treatment of patients who become infected when hospitalised. The possibility of Sepsis, hospital-acquired Clostridium difficile or nosocomial infections is increased by the lack of or suboptimal hand washing.
Deep learning and machine vision can track the hand hygiene of clinicians and surgeons using video footage and depth sensors. An Intensive Care Unit (ICU) leverages the support of machine vision to detect the appropriate time when the patient might need a mechanical ventilator or automated surveillance of vital signs.
Using these algorithms in healthcare can also predict post-surgery complications like hospital death, kidney failure, bleeding and requiring re-admission to the hospital, which are difficult for doctors to predict.
Administration work at hospitals like scheduling appointments, nurse call lights and billing systems are dealt with easily without much manpower and therefore it becomes easy for the personnel to concentrate on the more important tasks with patients.
The machine learning systems can also completely scan the patient record and provide recommendations to the doctor as well as rapidly analyse medical images and scans for accurate decision making.
AI can be used in healthcare for every part of its operation – organizing patient records, suggesting diagnoses via bot interaction, identifying patients through facial recognition, interpreting CT scans and operating room workflows.
In the process of ‘democratization’ of healthcare, power has slowly shifted from the physician to the patient. Patients can now get their lab results data or Electrocardiogram (ECG) on their phone, they can then analyse the results through an app on their phone and get the diagnosis even before a visit to the doctor. Anyone can perform multiple physical examination of their vital signs, eyes, ears, throat, heart and lungs through their smartphone applications. Access to Electronic Health Records (EHRs) resulted in patients’ reporting better medication adherence and many doctors becoming wary of the language used in the notes.
Applying AI in the prediction of life expectancy of terminally-ill patients can improve the accuracy of determining the time needed for care. Even though it was called the ‘dying algorithm’, the positive side is to make the life of patients and their carers easier and rewarding.